Chronic pain affects more Americans than heart disease, cancer, and diabetes combined. Yet, despite being the most common health condition in the United States, and having a $1T economic burden, it remains dramatically underfunded, underrecognized, and stigmatized. In contrast, diseases like Alzheimer’s, Parkinson’s, and cancer receive significantly more attention, research dollars, and media coverage. Why is that? And what can we do about it?
The Numbers Don’t Lie
According to the CDC, over 51.6 million U.S. adults live with chronic pain, and 17.1 million suffer from high-impact chronic pain that limits their daily life and work activities (CDC, 2023). In contrast:
• Alzheimer’s affects about 6 million Americans (Alzheimer’s Association, 2024)
• Parkinson’s: around 1 million (Michael J. Fox Foundation)
• Cancer: approximately 18 million Americans are living with or beyond a cancer diagnosis (American Cancer Society, 2024)
Despite this, chronic pain remains grossly underfunded. In 2012, NIH allocated just $396 million to pain research, about $4 per patient. Compare that to $431 per cancer patient and $97 per Alzheimer’s patient (NIH Categorical Spending Report).
More Recent Numbers: Some Progress, But Still Behind
Thanks to growing recognition of the opioid crisis and the need for better pain solutions, the NIH has increased pain research spending, primarily through the HEAL Initiative. Since 2018, HEAL has allocated over $1.5 billion to research on pain and opioid misuse (NIH HEAL Initiative). In 2023 alone:
• NCCIH requested $66 million for pain research (NCCIH FY23 Budget)
• NIAMS supported 31 pain research projects with over $5 million in funding (NIAMS Update, 2023)
While this marks progress, chronic pain still receives less funding per patient than other conditions.
Why the Discrepancy?
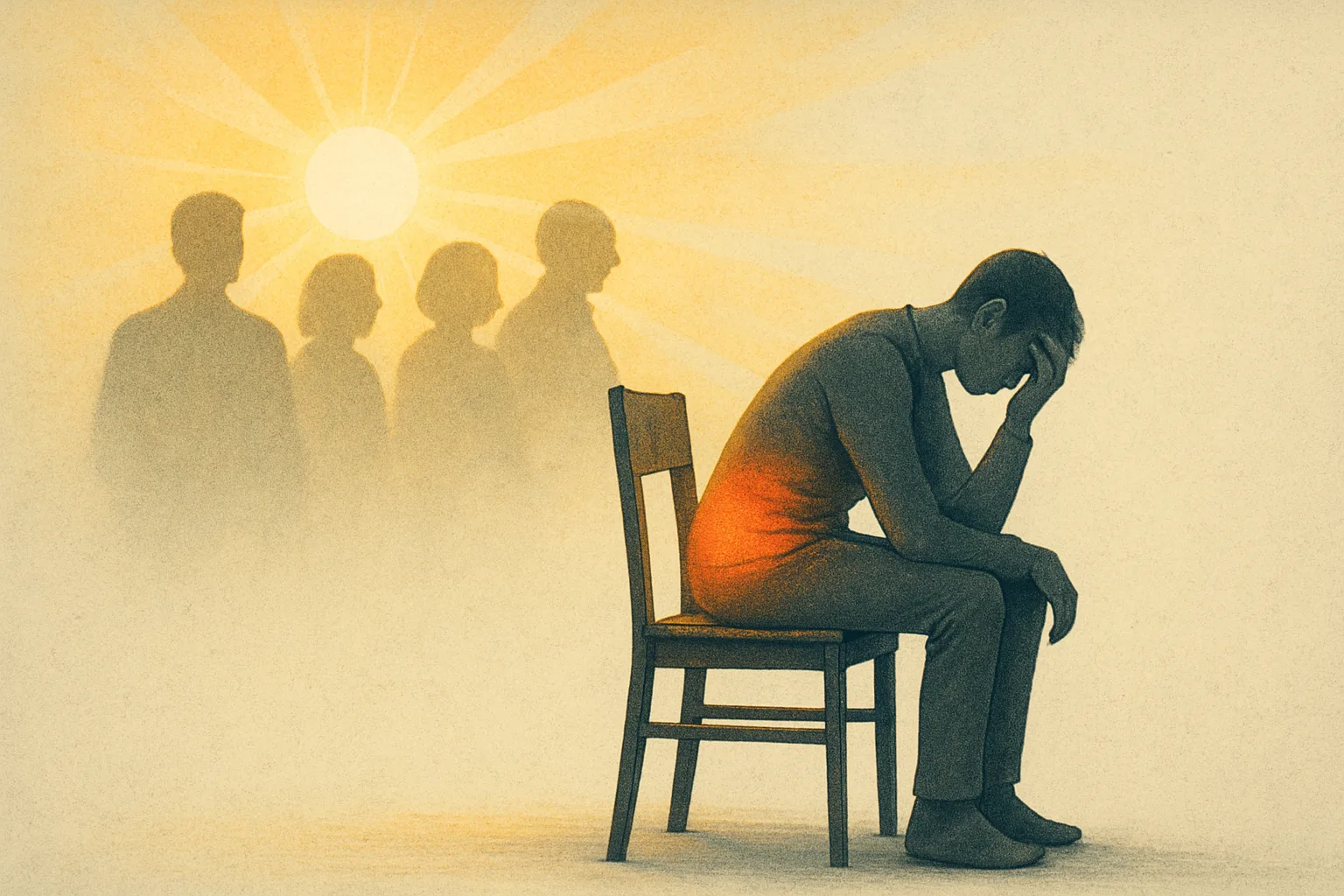
1. Invisibility & Stigma: Chronic pain is subjective and often invisible. Without visible symptoms, it is harder to communicate its severity, and patients are often met with skepticism.
2. No “Death Count”: Pain doesn’t usually kill people directly. It “just” ruins lives. Diseases with high mortality rates tend to get more attention and urgency from media, policymakers, and donors.
3. Fragmentation: Unlike cancer or Alzheimer’s, chronic pain isn’t a single disease with a powerful advocacy group. It’s a collection of conditions that often fall between medical specialties.
4. Opioid Backlash: The opioid epidemic made pain politically toxic. Public discourse shifted from helping pain patients to preventing addiction—sometimes at the expense of those who actually need relief.
What Needs to Change?
• National Campaigns: Launch high-profile public awareness efforts like those for breast cancer or Alzheimer’s. September is Pain Awareness Month—let’s make it matter.
• Increased Research Funding: Pain research deserves its own “moonshot”. Create dedicated NIH funding streams or even a Pain Institute.
• Stronger Advocacy: Unite pain-focused groups under one national banner. Get celebrity ambassadors. Go viral. (Remember the ALS Ice Bucket Challenge?)
• Better Policy: Enact legislation like the Advancing Research for Chronic Pain Act to improve federal data collection, funding, and pain care standards.
Conclusion
Chronic pain is the most common, most expensive, and most ignored public health crisis in America. The good news? We can fix that. With more awareness, funding, and political will, we can finally give chronic pain the attention it deserves—and improve the lives of tens of millions of Americans who live with it every single day. Innovations like Radiocaine, a groundbreaking imaging technology designed to visualize chronic pain, show that change is possible when science and awareness come together.
References
• CDC, 2023 Chronic Pain Data Brief
• Alzheimer’s Association, 2024 Facts & Figures
• Michael J. Fox Foundation – Parkinson’s Facts
• American Cancer Society – 2024 Facts & Figures
• NIH Categorical Spending Report
• NIH HEAL Initiative
• NCCIH FY2023 Budget
• NIAMS Pain Research Funding 2023